24 Feb 2022 Stroke evaluation by determination of high stenosis, occlusion, and emboli detection
TCD for Stroke Risk Evaluation and Management
Cerebrovascular ultrasound provides real-time information about the blood flow in addition to the hemodynamic changes as a result of various physiological as well as pathological states.
TCD can predict stroke by determination of high blood flow velocities, which allows indirect conclusions on stenosis or occlusion.
Frequently early stages of stenosis are not detectable because they become notable not before the grade of narrowing exceeds more 50% (ICA > 70%). Additional measurement of narrowing is restricted since increased BFV can also rely on hyperperfusion, which can be caused by disturbed cerebral autoregulation. Thus, detection of intracranial vascular stenosis for stroke risk evaluation relies largely on indirect criteria.
Pathology
Atherosclerotic processes are in a majority of cases the reason of intracranial occlusions which can lead to stroke. In contrast to that, intracranial increase of blood flow velocity can rely on different reasons, which efforts a note of caution in differential diagnostic considerations: E.g. vasospasm after subarachnoidal haemorrhage, autoimmune or infectious vasculitis, isolated atherosclerotic narrowing caused by diabetes, hypoplasia of single vessel segments, anemia and vascular dissection are frequent reasons of BFV accelerations.
TCD – diagnostic examinations
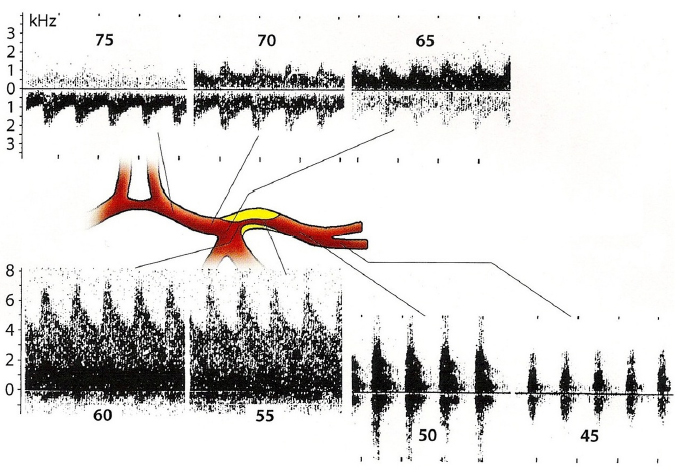
1. Diagnosis of extracranial carotid artery stenosis
Using TCCD > takes advantage due to imaging of plaque morphology while TCD is more sensitive in determining blood flow velocity.
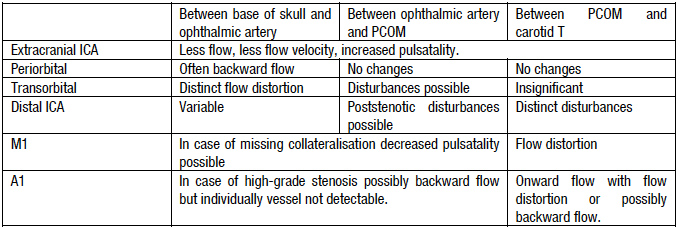
2. Diagnostic criteria of high-grade stenosis (> 70%) in intracranial carotid artery (ICA)
Modified from “Doppler- und Duplexsonographie der hirnversorgenden Arterien”, Tab. 16.2, Widder et Görtler, Springer Verlag, 6. Auflage.
Diagnosis of stenosis of distal ICA within the carotid siphon seems to be technically difficult since in usual examination depths of 60 to 70 mm signals of different vessels are detectable (ACOM, PCOM, P1, sometimes contralateral segments), which can imitate stenosis originally generated by turbulent collateral flow signals. Neuronavigated TCD could help to minimize this problem since it allows even an estimation of each insonation angle and visualisation of the vascular tree.
3. Diagnostic criteria of MCA stenosis
Because of the smaller diameter of MCA (2.0-2.5-3.0 mm) Digital Subtraction Angiography (DSA) does not allow the estimation of MCA stenosis. Up to now these narrows can only be determined by measurement of BFV.
Stenosis less than 40% (120-160 cm/s) are characterized as “low grade”, 40-70% (160-220 cm/s) as “medium” and more than 70% (≥ 220 cm/s) as “high-grade”. Possible hyperperfusion needs to be excluded prior to diagnosis. Therefor, it is necessary to determine the Lindegaard-Ratio (vMCA/vICA). Values less than 2 point to the presumption of hyperperfusion rather than stenosis. In contrast to that, values higher than 3 as well as BFVs higher than the double normal velocity presume stenosis firstly.
Likewise, comparison of pre- and poststenotic BFVs as well as bilateral velocity comparison provides useful information.
Modified from “Doppler- und Duplexsonographie der hirnversorgenden Arterien”, Tab. 16.2, Widder et Görtler, Springer Verlag, 6. Auflage.
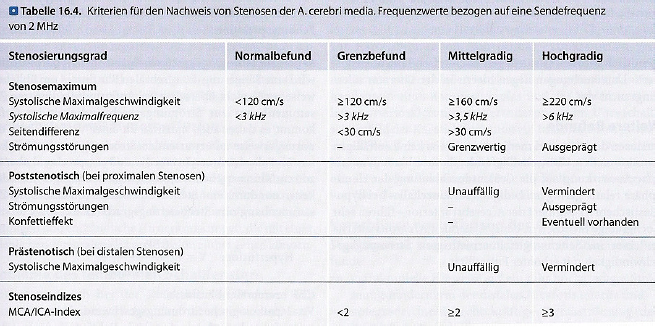
High-grade stenoses in the segment of proximal MCA in a patient suffering from TIA.
From: Doppler- und Duplexsonographie der hirnversorgenden Arterien, Tab. 16.2, Widder et Görtler, Springer Verlag, 6. Auflage.
4. Stenoses of the ACA
Doppler sonographic findings in the A1 section of the anterior cerebral artery are highly variable and depend initially on the degree of stenosis of the internal carotid artery. If this is not yet high, the anterior cerebral artery is usually perfused antegrade. In the case of carotid T stenoses, post-stenotic flow disturbances are also found. In the case of high-grade stenoses in the carotid siphon, however, the anatomical situation in the R. communicans anterior is decisive. If this is well developed, there is regularly retrograde flow through the anterior cerebral artery. In the other case, the anterior cerebral artery can usually not be visualised or can only be drained with a strongly reduced flow.
5. Diagnostic criteria of PCA stenoses
Outflow stenoses of the posterior cerebral artery are relatively common. It is not uncommon for this to be a residual finding in partially recanalised transit thrombi of the vertebrobasilar vascular system.
Due to the numerous anatomical variants, occlusions of the posterior cerebral artery can only be diagnosed with uncertainty. The same applies to the anterior cerebral artery. Isolated stenoses of the posterior cerebral artery, on the other hand, can often be recognised by the typical flow abnormalities.
Problems
- False negative results caused by poor ultrasonic bone windows
- Difficult differentiation from hyperperfusion
- Confusion caused by mistaken vessel labelling in depth of > 55mm
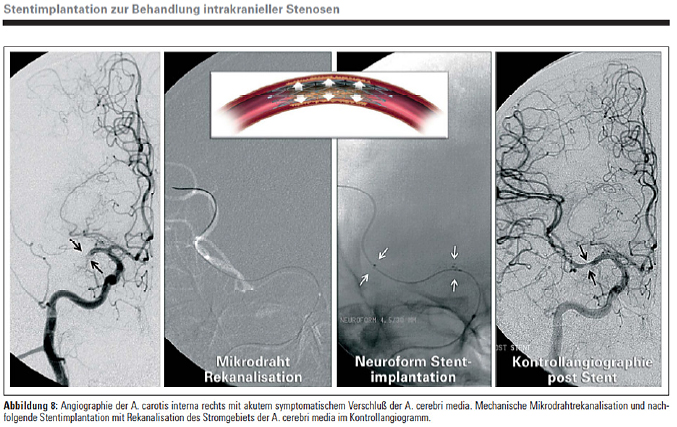
Stroke treatment
Paramountly, the most important preventive measure is to reduce atherosclerotic risk factors.
That means abstinence from smoking, adequate treatment of hypertension, hypercholesterolemia and diabetes as well as reduction of obesity.
The therapy of intracerebral vessel narrowing is depending on the grade of stenosis as well as neurological complications.
The guideline of the German Association of Neurology concerning “cerebral ischemia” regards in case of asymptomatic stenosis or TIA as initial manifestation the treatment with 100-300 mg acetylsalicylic acid per day. With the occurrence of neurological recurrent symptoms, angioplasty and, if possible, stenting is indicated for anterior circulation; additional to acetylsalicylic acid and Clopidogrel (grade of evidence C).
Because of introduction of intracerebral angioplastic procedures (2002), the value of bypass surgery becomes less important.
From: Stentimplantation zur Behandlung intrakranieller Stenosen Klein GE, Zeitschrift für Gefäßmedizin 2007; 4 (1), 4-10.