10 Jan 2022 Persistent Foramen Ovale (PFO) diagnostic
TCD-based PFO test for detection of stroke risk
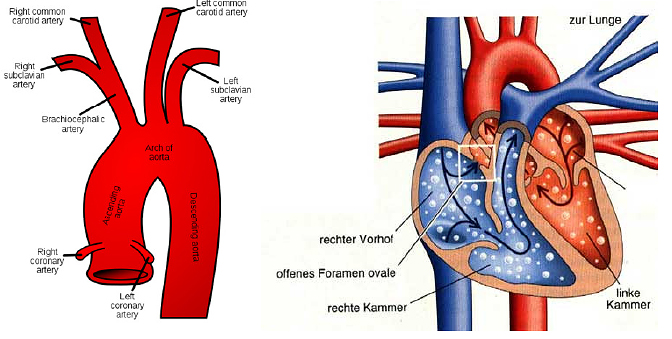
Heart failures like atrial septal defects (ASD) as well as ventricular septal defects (VSD) can be detected by TCD measurement.The most common and well known septal defect is a Patent Foramen Ovale (PFO) causing Right to Left Shunt (RLS). RLS are direct connections between right (pulmonary) and left (systemic) circulation. By this connection blood can cross to the other circulation without passing pulmonary capillaries.
PFO persists in approximately 25% of European population. In a sense, PFO is less considered as a defect but rather than a normal variation. The PFO is a bypass, which is necessary for fetal circulation. In patients suffering from PFO this bypass is not entirely occluded.
VSDs are the most common heart failure (3/1000 – male:female 1:1), which is often prominent and diagnosed very early. ASDs account for about 8% of heart failures, which often remain unnoticed. In adults they account for approximately 1/3 of all heart failures.
Pathology
Scattered emboli, which have its source from systemic circulation (e.g. embolic deep vein thrombosis), usually get stuck inside the pulmonary vessels. Depending on their size, this can be asymptomatic (autogenic emboli-lysis) or results in case of bigger emboli in sudden pulmonary embolism.
Providing a RLS, there is a danger that emboli cross directly into systemic circulation and result in organ infarction (paradox embolic event (PEE)). Cerebral stroke is the most feared PEE since cerebral ischemia is irreversible.
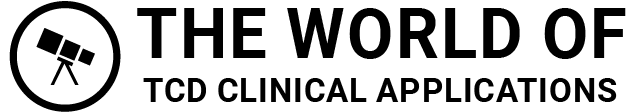
Truncus brachiocephalicus (with major braches: left A. subclavia and left carotid artery) as well as right A. subclavia and carotid artery are (despite coronary arteries) the first three branches of the aortic arch. The carotid arteries and vertebral arteries, which arise from both subclavian arteries, are the only brain feeding vessels. Depending on anatomy and little regenerative capability of brain tissue, these vessels are especially vulnerable to embolism.
In healthy subjects blood clots arise usually from left cardiac atrium or ventricle, which result from cardiac wall motion abnormalities (e.g. atrial fibrillation) or from bacterial colonisation in case of endocarditis.
Providing existing RLS, many other sources of emboli account as origin. Despite previously mentioned deep vein thrombosis also scattered tissue particles during surgery are possible. More frequently, reason for embolism are gasous bubbles, which reach the systemic circulation due to vacuum during surgery in sitting position (e.g. shoulder surgery or neurosurgery).
Usually, pressure within the systemic circulation exceeds pressure within pulmonary circulation, which inhibits blood to cross from right to left. Due to long persisting shunts pressure proportions may change (Eisenmenger syndrome).
However, in circumscribed situations, even in healthy subjects pressure in pulmonary circulation can exceed pressure in systemic circulation. That includes pressing for defecation, coughing or Valsalva maneuver, which is also used for diagnosis of RLS.
Particularly relevant become RLS for divers. Solved nitrogen may bubble up during surfacing. Usually these bubbles get stuck inside pulmonary arteries is exhaled immediately. In case of RLS these bubbles can cross to systemic circulation and may reach brain-feeding vessels, which can result in stroke depending on the amount bubbles.
Diagnosis of RLS using TCD
- Echocardiography (transthoracal (TTE) und transoesophageal (TEE))
- Contrast MRI
- Cardiac catheter examination
- Transcranial Doppler sonography
- In Germany, echocardiography is considered as gold standard, which is caused differently: Heart failures belong to the subject of cardiology and cardiologists are quite familiar with echocardiography. It offers the advantage that RLS can not only be detected but can be located as well. TEE is more sensitive as TTE. To perform TEE, it is usually necessary to sedate the patient, which is an invasive procedure.
- Also MRI can detect RLS but is quite expensive and cannot be performed in case of claustrophobic patients or metallic implants like cardiac pacemakers.
- Cardiac catheter examinations are very invasive procedures, which take risks. Although it is clinical routine, catheter examination are only performed in cases where other methods fail to demonstrate the proportion of RLS. Typical complications are: secondary bleeding at the injection site, vascular dissection and heart valve lesions.
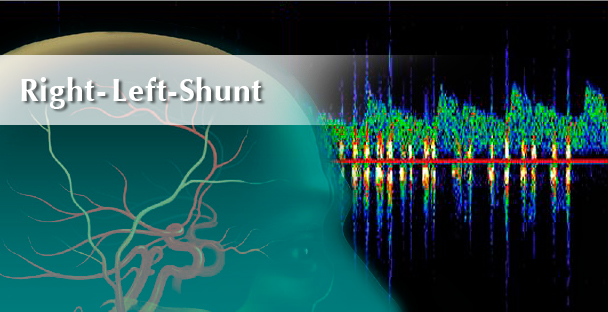
- TCD is the least invasive method to detect RLS, which can be applied without sedation and does not take the risk of complications (Cave: rare allergic reactions to US contrast agents). Moreover, it is the cheapest examination.
Studies suggest that detection of RLS by TCD is superior to echocardiography because TTE and TEE often reveal negative results (Martínez-Sánchez et al., 2011; Van et al., 2010; Sastry et al., 2009).
Specificity of TCD is nearly 100% and sensitivity between 85-95%. In contrast to TTE and TEE even extra-cardiac shunts can be detected.Due to little morbidity and little costs TCD seems to be well suitable for screening examinations in patients suspected of suffering from RLS. Thus TCD and TEE/TTE should be considered as complementary (Nedeltchev and Mattle, 2006)
RLS detection using TCD
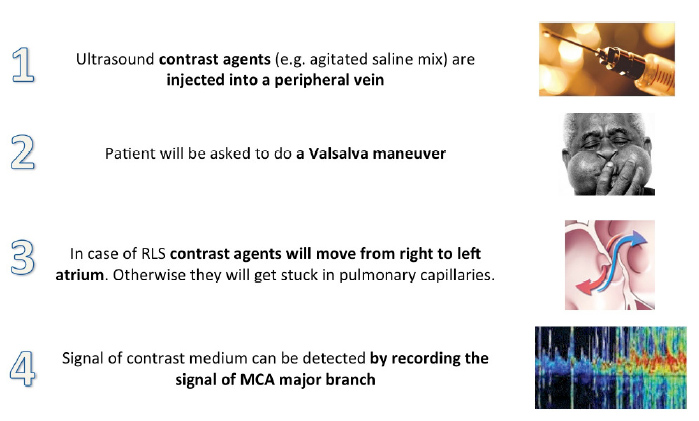
To perform TCD examinations an ultrasound contrast medium is necessary, which cannot pass pulmonary capillaries.
On the one hand a commercially available contrast medium can be use (e.g. Echovist©) on the other hand some authors recommend (because of relatively high costs) to use an agitated mix of 6-7 ml saline, 1-2 ml patient blood and 0.2 ml air. This mix should be agitated until a dense foam without macroscopic bubbles has been generated.
Cave: Pharmaceutical laws, FDA, etc. Depending on the country, at least informed consent is necessary.
Valsalva maneuver
While the patient keeps mouth and nose closed, he is advised take a deep breath and afterwards to exhale forcefully. This results in increased pressure inside the airways, which in turn increases pressure inside pulmonary circulation and thereby causes a pressure reversal across the shunt.